If there’s one bright spot in behavioral health policy right now, it’s this: Certified Community Behavioral Health Clinics (CCBHCs) are expanding. They’re connecting people to care faster. They’re easing pressure on emergency rooms. And they’re giving states a tangible way to build behavioral health infrastructure that lasts.
But behind that momentum is a looming question: will the funding hold?
As states move to expand their CCBHC programs, and more clinics transition from SAMHSA grants to Medicaid demonstrations, there’s growing concern about how long the federal support will last, and what happens if the rules change.
SAMHSA to Dissolve: Programs to Merge With AHA
In March 2025, the U.S. Department of Health and Human Services announced it would dissolve the Substance Abuse and Mental Health Services Administration (SAMHSA), merging its programs into a new umbrella agency, the Administration for a Healthy America (AHA).
That’s not a small change. SAMHSA helped design and launch the CCBHC model. It provided grant funding, technical assistance, and operational guidance that allowed hundreds of clinics to scale services across the country.
Now, with SAMHSA phasing out and many federal agencies in flux, providers are left with uncertainty. Oversight of the Demonstration Program is shifting. Points of contact are unclear. And the samhsa.gov domain is offline, meaning prior federal guidance is no longer accessible through official links.
For programs still relying on SAMHSA Expansion Grants—or preparing to join the Medicaid demonstration—the handoff is already creating friction. Delays in grant communications, a shrinking federal workforce, and limited updates on technical aid are raising concerns.
But for all the uncertainty around who is in charge, the why behind CCBHCs hasn’t changed.
What Makes CCBHCs Different
At their core, CCBHCs are built to meet people where they are. Same day appointments. 24/7 crisis response (such as mobile crisis teams). Integrated care for people with serious mental illness, substance use disorders, and complex needs. This model wasn’t built to check a box. It was built to solve gaps in care.
CCBHCs provide more than therapy or medication management. They also provide:
- Peer support from specialists with lived experience
- Housing navigation
- Care coordination across justice, health, and social systems
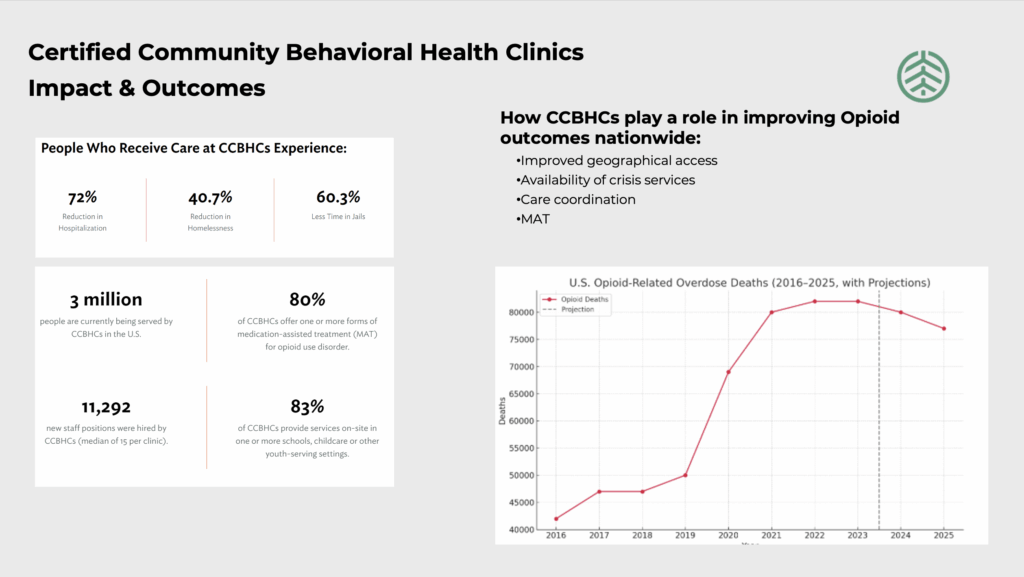
And because they’re required to report on outcomes, the data is starting to tell a clear story: the model is working.
A 2023 analysis by the National Council for Mental Wellbeing found that Certified Community Behavioral Health Clinics helped reduce hospitalization and ER visits, while increasing access to care and workforce capacity, especially in rural and underserved communities.
And they’re expanding access to substance use care at a time when demand has never been higher. Nearly 90% of CCBHCs now offer at least one form of medication-assisted treatment (MAT) for opioid use disorder, compared to just 64% of other facilities. Two-thirds have seen MAT engagement increase since becoming a CCBHC, with nearly a third reporting jumps of 20% or more.
As of May 2025:
–18 states are part of the CCBHC Medicaid Demonstration Program
-Over 500 clinics are running nationwide
–10 more states are preparing to join in 2026
That kind of growth is rare in Medicaid funded care, especially when it comes with bipartisan support and measurable outcomes.
Where Do Crisis Stabilization Units Fit In?
Crisis Stabilization Units (CSUs) are a core part of behavioral health that CCBHCs help support. These short-term, community-based programs offer immediate care for individuals experiencing mental health or substance use crises, serving as an alternative to emergency departments or inpatient care. By integrating CSUs into CCBHC networks alongside mobile crisis teams and 24/7 access lines (like 988), states can provide more responsive, cost-effective care that prevents unnecessary hospitalization and connects people to long-term care.
More than 80% of CCBHCs are already partnering with 988 call centers, well ahead of federal targets. And nearly a third added mobile crisis response capacity as a direct result of becoming certified.
Certified Community Behavioral Health Clinics are evolving into the front door of a better crisis care system. But that kind of impact depends on flexibility and funding. And both are facing serious pressure.
It May Not Be Enough for Certified Community Behavioral Health Clinics to Keep Their Funding
Earlier this year, SAMHSA opened the next round of applications for states to join the Certified Community Behavioral Health Clinic demonstration program. It’s a big opportunity, and a big lift.
At the same time, the Centers for Medicare & Medicaid Services (CMS) have begun signaling that it may narrow what qualifies for federal Medicaid match. There’s been talk of tightening the definition of “medical necessity,” a change that could quietly exclude key CCBHC services from reimbursement.
The impact? Services like housing, employment support, and peer engagement, essential to recovery but not always considered “clinical,” could lose funding. And if that happens, states may have to scale back what CCBHCs can offer.
That’s not just a technical adjustment. That’s a huge structural shift in the services programs can provide to communities.
What to Keep an Eye On
1. Match Rate Volatility
CMS may limit what counts toward federal Medicaid match, potentially excluding non-clinical services like care coordination, peer support, and housing navigation. This would shift the financial burden to states, many of which are already managing tight budgets.
2. Grant Expiration Pressures
Many providers still rely on SAMHSA Expansion Grants, which are time limited. Without a state demonstration waiver in place, or if match eligibility narrows, those providers could lose core program funding just as community reliance grows.
3. State Infrastructure Gaps
Even for states moving into the Demonstration Program, building the backend infrastructure is a heavy lift. States must stand up rate structures, billing systems, data tracking, and outcome reporting with limited time and technical ability.
Our Take: Flexibility Is Key
CCBHCs power comes from flexibility, giving providers room to respond to local needs and letting states build solutions that work in the real world.
Cutting funding for non-clinical services not only limits flexibility; it risks unraveling the very support that makes this model work.
We know these programs help people stay well, stay housed, and out of crisis. That’s not just a policy win; it’s a systemic shift for communities. But it only works if providers can keep doing what works.
What You Can Do Now
1. Talk to your state
Make sure Medicaid agencies understand what’s working, and what you need to keep delivering services.
2. Watch CMS guidance
Stay alert to rulemaking on DSHPs, DSIPs, Section 1115 waivers, and match definitions.
3. Share your outcomes
Whether its ER diversions, reduced hospital stays, or better recovery retention, document and share your outcomes. Policymakers need stories backed by data. Provide what you can.
Radicle Health Is Watching Closely
We’re tracking demonstration expansions, AHA announcements, and every Medicaid rule that could affect funding or flexibility for CCBHCs.
If you’re navigating this transition, or worried about what’s next, you’re not alone. We’ll keep asking the right questions and bringing you answers that help.
Stay up to date with us here.