Behavioral and mental health services EHR systems are evolving—becoming more integrated, proactive, and holistic every year. This shift benefits clients and boosts practice efficiency but keeping up means having the right technology in place to support these changes.
Today’s clients expect more: client portals, Telehealth options, and flexible payment methods. Behind the scenes, agencies are working smarter and collaborating across care teams to provide integrated care. These changes are reshaping the client journey—and your Electronic Health Record (EHR) software is at the heart of it all. It tracks every step, from no-shows to clinician notes, giving you the data you need to uncover insights and improve processes.
That’s why many organizations are rethinking their EHRs. They’re looking for solutions that are more adaptable, scalable, and cost-effective.
This guide is designed to help behavioral and mental health leaders navigate a seamless transition to a new EHR software platform. Inside, you’ll find:
- How EHRs have evolved over time
- Key signs it’s time to upgrade your system
- Features that can deliver the most value to your practice
- How to get your providers on board with the switch
- Steps for a smooth and strategic transition
- Real success stories from practices that made the leap
Ready to reimagine what your EHR can do? Let’s get started.
What are EHR Systems? Then vs. Now.
EHR systems have come a long way. What started as simple digital client charts—a big improvement over handwritten notes—has evolved into a powerful agency management tool. Traditionally, EHRs (also called EMRs) securely store critical data like:
- Provider notes
- Reports and assessments
- Demographic data
- Billing information
- Treatment plans
Today’s EHR systems can do so much more. Thanks to innovations like cloud computing modern EHRs don’t just store information—they adapt and scale to meet your organization’s changing needs. Today’s top EHR systems go beyond storing information to flex and scale as your needs shift.
Here’s how top EHR systems support behavioral and mental health agencies today:
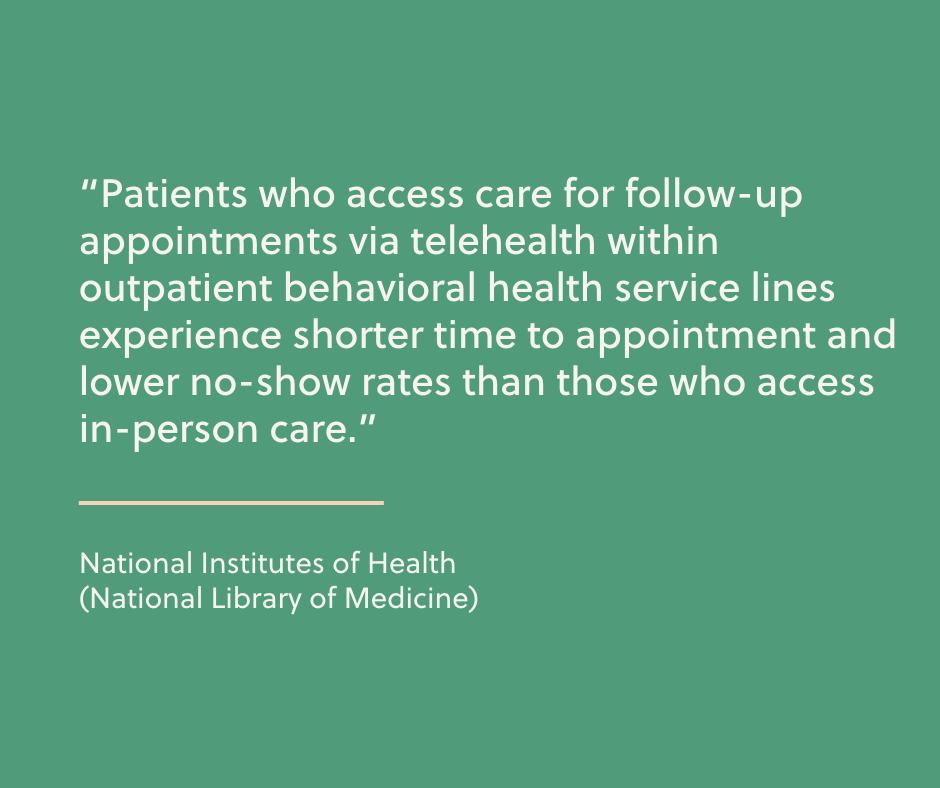
- Empower clients: Give clients more options, like records access, self-scheduling and telehealth, improving their experience and satisfaction.
- Save time on repetitive tasks: Reduce the manual work required for scheduling, documentation, and billing so staff can focus on clients.
- Provide all-in-one tools: Eliminate the need for multiple systems by including communication, billing, and service delivery features in one platform.
- Support continuous improvement: Provide tools to easily track and analyze key metrics, helping agencies spot opportunities to improve.
- Make compliance easier: Simplify the audit process with organized, accessible records.
Modern EHRs are no longer just digital filing cabinets—they’re now essential tools for improving how your organization operates and how you care for your clients.
Signs it’s Time for an Upgrade to your EHR Software
Your EHR software should make life easier for everyone—front office staff, providers, clients, and your revenue team. But if any group is struggling at any stage of the client journey, it might be time to document these challenges and their impact. This can give you a better understanding of what you may need to change.
Here are common red flags that signal your EHR system may be holding you back:
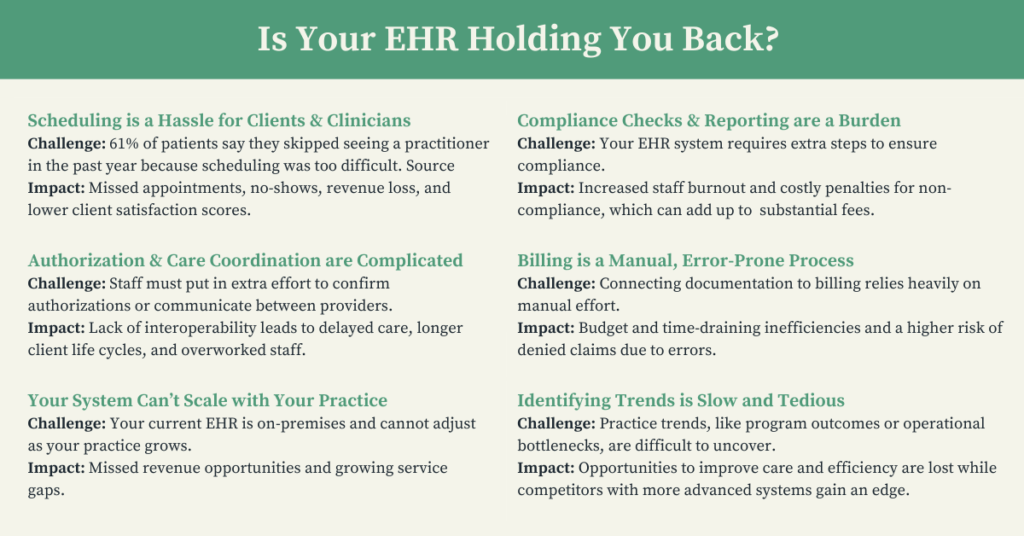
These challenges are just the beginning. Identifying the obstacles your staff faces every day will help ensure your next EHR system is the right fit—one that truly meets the needs of your team and clients.
What the Top EHR Systems for Behavioral Health Offer
The features you need today might not be the ones you’ll need tomorrow—recent years have taught us that flexibility is key. A secure, cloud-based EHR system allows you to adapt to client trends, regulatory changes, and unforeseen challenges as they arise.
Every behavioral health practice is unique, but a modern EHR system designed for mental health care should offer these essential features:
- Data exchange and integration to meet the 21st Century Cures Act requirements.
- Reporting and analytics to track trends and support evidence-based care.
- HIPAA-compliant Telehealth capabilities that are built into the platform.
- Visit documentation that is comprehensive and easy to manage.
- E-signature capabilities to simplify processes for clients and staff.
- Integrated billing tools tied directly to documentation for greater accuracy.
- Coding support to reduce errors and speed up claims.
- Robust security to protect sensitive client information.
- Built-in compliance tools to ensure regulatory standards are met.
- User-friendly interfaces that make workflows intuitive and accessible for all staff.
- Ongoing support from the EHR provider during training and beyond.
When it comes to EHR configurability, it’s less about choosing a big-name brand and more about finding a system purpose-built for mental and behavioral health. Well-designed solutions take industry-specific needs into account, helping you improve efficiency and client experiences right out of the box.
Wondering How to Afford an EHR?
Our FREE planning worksheet helps you figure out how an EHR can fit your budget!
Getting Your Team on Board
Introducing new software can be a delicate process, especially when getting your team to buy in. Adopting a new EHR will require training, time for staff to adjust, and patience before you see a return on your investment. But involving your team early on makes all the difference.
The first step is to involve key providers and administrative staff in the selection process. Their input ensures that the new system meets your agency’s needs and helps build excitement for the transition.
Establish a capabilities baseline. Ask your team these key questions to understand what they need:
- What are you trying to do but can’t with the current EHR?
- How do these limitations affect you, your department, and (if applicable) the organization as a whole?
- What’s working well that you’d like to keep?
Creating a Transition Team
Involve a mix of stakeholders to ensure the transition works across your organization for all participants. You make want to include:
- Executive Leaders: Help tie technology decisions to the organization’s vision and high-level goals. They’ll ultimately authorize decisions, build consensus, and drive the process forward.
- Clinical or Program Directors: Experts in how the EHR aligns with clinical and service needs, workflows, and audit-critical data.
- QA: Focused on reporting capabilities, compliance, and identifying opportunities for improvement.
- Administrative Staff: Can act as early testers and trainers, providing feedback on usability and workflow integration.
- Billing and Grant Writing Staff: Can evaluate the system’s ability to support service data analysis and funding needs.

Getting your team on board isn’t just about selling them on the new system—it’s about making them part of the process from the start. Their input, insights, and feedback will help ensure the transition goes as smoothly as possible.
Steps for a Smooth Transition to Your New EHR
With your Transition Team in place and your new EHR system selected, it’s time to create a roadmap for implementation. Partner with your in-house specialists to map out clear milestones, assign responsibilities, and ensure shared ownership of the process.
Step 1: Preparation & Configuration
Prepare a clear message for administrators and providers who are not on the Transition Team to give them a healthy heads-up about the new EHR. Be sure to highlight:
- Who’s involved: Introduce the Selection/Transition Team and their role.
- Why it matters: Highlight the specific problems the new EHR will solve for the organization, each department, and individual roles.
- Key dates: Share timelines for questions, training sessions, and implementation
- Prepare records for migration
- Organize and clean up records to ensure they’re ready to move.
- Pull reports of current key performance indicators (KPIs) to compare with future results after the transition
- Identify areas for improvement including:
- Redundant tasks that can be eliminated.
- Workflows that can be simplified.
- Gaps in interoperability that need to be addressed.
Let clients know about the upcoming change. Be transparent about:
- Timelines: When will each stage of the new system roll out?
- Benefits: How will this change improve their experience?
- Support: Where can they go with questions?
Step 2: Implementation
- Assign roles like Staff Login Lead, QA Lead, and Internal Help Desk to keep the process organized.
- Perform test runs to identify and resolve any migration issues before rolling out changes to the rest of the staff.
- Create a backup plan to ensure service delivery and billing can continue smoothly during the transition.
- Migrate client data into your new EHR’s database.
- Perform QA testing to ensure that the new EHR system is working and running as expected.
- Consult your EHR’s support staff for any questions along the way.
Step 3: Adoption & Beyond
- Tap your most engaged staff members to train others and answer questions.
- Gather tips from your team as they find efficient ways to navigate workflows in the new system. Share these insights widely.
- Continue using your EHR provider’s resources to address questions and offer ongoing assistance to clients adjusting to the new system.
- Set a date to compare your new KPIs with your baseline. Use these insights to adjust workflows and refine processes for even better results.

Getting an EHR System Upgrade: Real-World Stories
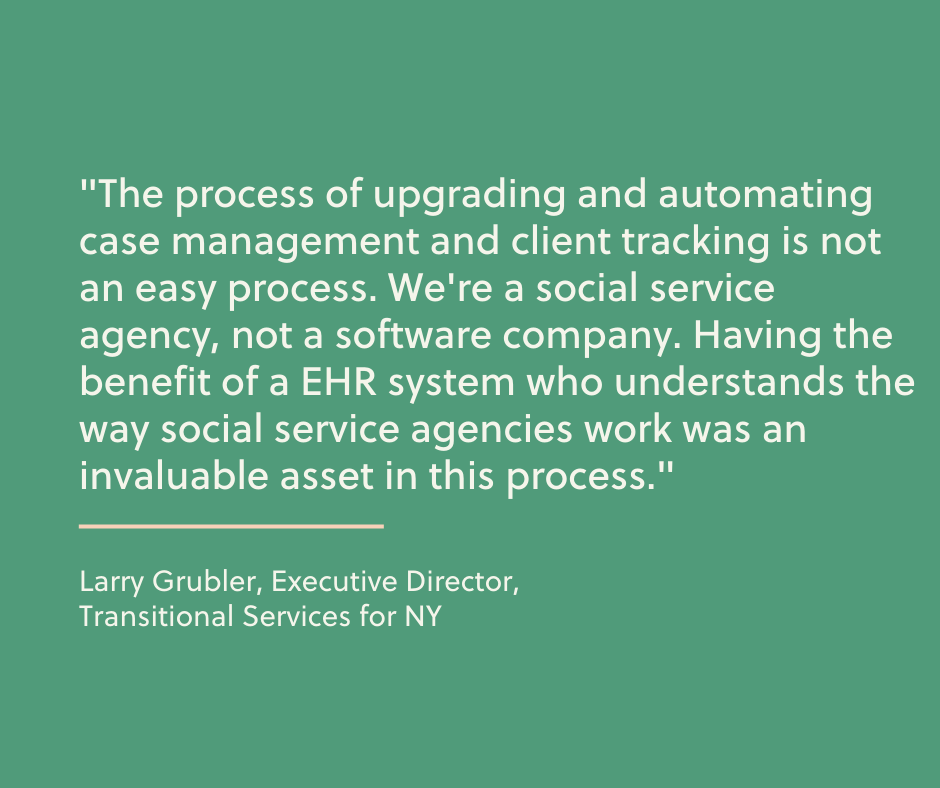
Sometimes, the best way to understand the impact of an EHR upgrade is to hear how others have navigated the process. Here are three organizations from Radicle Health companies that transformed their operations and client care with the right EHR system:
Graduating to an accurate, real-time picture of client care:
New York-based Rehabilitation Support Services (RSS) faced a major data visibility challenge. They needed a clear dashboard showing both the services clients had received and the ones they were eligible for. Instead of wasting time digging through data, their new EHR provided the holistic view they needed, letting them spend more time helping clients.
Paving the way for painless audits and “the best partnership [they’d] ever been a part of”:
DePaul Community Services dealt with data chaos: dozens of funding streams, multiple systems, and operations spread across counties in two states. After switching EHRs, they eliminated duplicate entries and shortened information retrieval time from days to just 5 seconds. They also described the implementation process as “the best partnership [they’d] ever been a part of.”
A smooth implementation, within budget, in a single business quarter.
A Better Way, a California non-profit supports children and families—but their old EHR system wasn’t supporting them. Within just three weeks of implementation, they understood their new EHR better than the one they’d been using for three years. By working closely with their implementation team, they customized workflows and reports that solved pain points and helped them achieve their goals.
Read the A Better Way case study
Next steps
Switching to a new behavioral health EHR is a significant decision, but it doesn’t need to feel overwhelming and can be minimally disruptive to your practice’s daily operations. When approached strategically—and with your staff’s active engagement—the transition can lead to meaningful improvements within weeks of implementation.
The right EHR Systems can:
- Reduce time spent on repetitive tasks, making workflows easier for your team.
- Close gaps in service delivery and enhance the client experience.
- Automate compliance and reporting, saving time and minimizing stress.
- Empower your agency to analyze data and identify trends that drive better outcomes.
These improvements keep your practice competitive and allow you to provide the highest level of care to your current clients while preparing for future growth.
Whether you’re considering a switch or just exploring your options, we’re here to help. Learn more about Radicle Health’s EHR Systems here.
And if you’re wondering how to make your EHR upgrade more affordable, we’ve got you covered. Download our guide, “How to Afford an EHR System Without Breaking the Bank,” to learn:
- How to break down EHR costs and identify hidden fees.
- Federal and state funding opportunities to offset expenses.
- Ways to maximize ROI through training, planning, and ongoing improvements.
Get your free guide now and take the first step toward a smarter, more cost-effective EHR transition.